Results
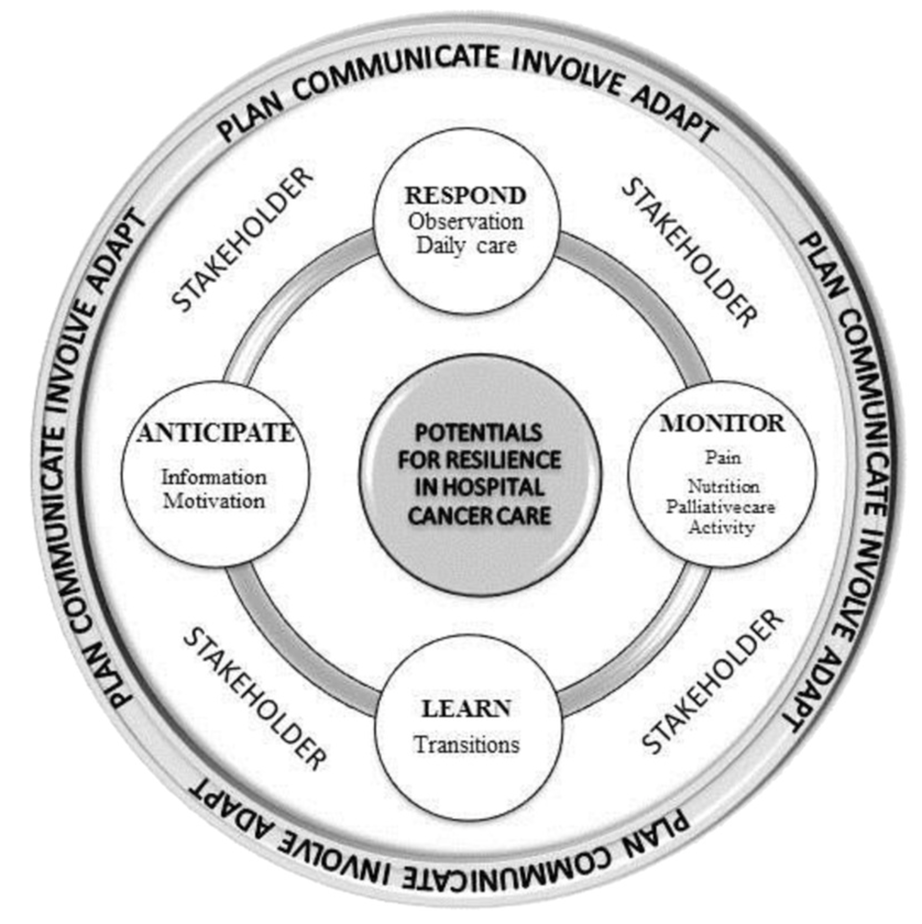
The results are presented according to the RHC framework and the four potentials for resilient performance.15,16,22 Under each heading, we include mechanisms where next of kin contribute as resilience-shaping factors.
The Potential to Respond
Next of Kin's Ability to Observe Guides Care Decisions-Makers' Response
The health professionals in this study highlight next of kin as important stakeholders in helping them respond more quickly to change in patient condition, because of their observations. Results show that healthcare professionals do not always know if it is safe for the patient to go home between treatments. If the patients, e.g., live with their next of kin, they are more likely to be discharged because they have someone who can observe and respond in case of adverse events such as fever, bleeding, or other discomfort related to the treatment or illness. In these situations, next of kin are often referred to as equally or more important than other healthcare personnel in the municipality.
We discharge many patients who are very ill. For example, when there is a compression fracture in the column, we are afraid of threatening cross-sectional lesion or patients on chemotherapy that have to come to the hospital rapidly if they experience fever. They [next of kin] are widely utilized. It is very often that we miss it when next of kin are not present.
(Consultant, hospital A)
Next of kin often guide healthcare professionals in making care decisions. The findings show that observations from next of kin provide important knowledge and insight into how capable the patients are of handling the burden and adverse effects of treatment. When next of kin are involved, they often give healthcare professionals important information that can help understand the patient's condition. This information can be crucial for deciding further treatment or changing the care plan.
Lastly, I participated in rounds with a preterminal patient,who, even though she was awake and perceived as being clear and oriented, did not make sense of pain. She had a serious infection and pneumonia, and we tried to ask her if there was a change in the condition concerning cough or breathing. Then the husband could tell us that her breathing had become worse and that he felt she was breathing more heavily. This happens quite often.
(Consultant, hospital A)
Dependency of Next of Kin in Daily Care to Respond Quickly
Managers and healthcare professionals claim to depend on next of kin to give the patient safe and high-quality care. Next of kin perform important care tasks, e.g., if the patient needs to be fed or is uncomfortable. These tasks often require the staff to be with the patient for a long time. On shifts with low staffing, next of kin are often the “pieces of the puzzle” that help managers and staff complete all tasks required of them by internal and external stakeholders (e.g., other patients, management, wards, or colleagues). This next of kin empowerment enables the staff to respond more quickly to patients who do not have their next of kin at bedside.
The Potential to Monitor
Next of Kin Watch Over Medication and Nutrition in Patient Care
The next of kin are assigned daily tasks either by the patient or healthcare professionals related to monitoring the patient's medication for pain treatment, nutrition, and daily care.
They [next of kin] often help to transport the patient, follow the patient to take blood samples, check the medical list, and also ensure that the patient takes the medication at the right time, especially if the patient doesn't want homecare. They inject medications, measure temperature and contact the hospital if the patient experiences fever. They [next of kin] have a huge sense of responsibility he patient and are resource persons for the patient, us (hospital), and the municipalities.
(Nurse, hospital A)
Healthcare professionals describe how next of kin have in-depth knowledge about the patient including how he/she was before the cancer diagnosis. For example, if the patient had poor appetite, a next of kin will sometimes know better than a nurse what the patient would eat and is often a good resource in encouraging the patient to eat.
Next of Kin Oversee Patient Activity Level
Physical activity and rehabilitation before new treatment are another area where next of kin's ability to monitor the patient is highlighted. Next of kin are often considered to have the capacity and motivation to contribute something extra during patient visits. Healthcare professionals often suggest that next of kin can help the patient with daily activities or physical activity by, e.g., taking the patient for a walk. In the hospital, this should be voluntary, but when the patient is at home between treatments, the expectation of next of kin's contribution to daily care is more explicit.
Watching Patient Signals in Palliative and Terminal Care
Healthcare professionals note that next of kin often are important partners in monitoring palliative and terminal care. Next of kin's involvement seemed to be more obvious and legitimized in this area. Healthcare professionals often work in close collaboration with next of kin in terminal care. In this stage, healthcare professionals learn and inform next of kin what to look for in the patient's condition, how to care for the patient by, e.g., moisturizing the mouth or observing if the patients are in pain or discomfort. The next of kin's perceptions are considered when the patient's condition changes. Healthcare professionals and next of kin often have different views and expectations of what is in the patient's best interest. This disparity is most pronounced in what poses a potential risk to the patient. A lack of involvement of next of kin perceptions and expertise may result in an adverse outcome:
Then one evening the patient became very ill. There was a lot of medication and people all over the place. The problem was not lack of resources. The next of kin perceived that the patient was dying, and she probably was. This was not conveyed. There was so much turmoil that they [next of kin] felt overlooked. They went home. That night the patient died alone.
(Consultant, hospital B)
The Potential to Learn
Key Role for Safe Transitions Across Care Levels
As we saw in the next of kin potential to monitor, the potential to learn highlights next of kin's experiences and perceptions of the patient condition as important features of the hospital's ability to provide safe cancer care. Results show that the next of kin have a key role that cannot be fully replaced by other stakeholders or hospital staff in terms of making sense of experiences for safe transitions and incorporating informal learning processes between service levels. Next of kin contribute to healthcare services by helping the patient between home and hospital and with transfers between care levels within the hospital. Next of kin often hold and share important experiences that help healthcare professionals in improving their services by learning more about the patient's previous condition and history. Healthcare professionals describe the importance of continuity of care among healthcare professionals for building a close and collaborative relationship among all stakeholders to adjust and learn from next of kin's perceptions and experiences.
I think it's an assurance for next of kin that they meet the same nurses. Next of kin seem to report more of the actual patient condition when they meet the same nurses.
(Quality manager, hospital B)
In addition, next of kin often take a questioning role and thereby contribute to stronger vigilance among the healthcare professionals about issues such as medications and injection rates. Results indicate that healthcare professionals may detect failures sooner and avoid adverse events because of reminders from next of kin.
The Potential to Anticipate
Next of Kin Are Foreseeing Possible Deteriorations and Treatment Consequences
In this study, the potential to anticipate is highlighted as an area for growth and more systematic investigation. This study finds two important mechanisms that are essential for the potential for anticipating: (1) how healthcare professionals involve next of kin to understand the possible consequences of treatment and care and (2) how healthcare professionals enable next of kin to foresee and handle adverse events and possible deterioration in the patient's health.
In the two hospitals, we found no systematic next-of-kin involvement or special training for next of kin even if they were performing tasks requiring special training and skills:
A next of kin approached me today and said, “We feel so alone in this. We control things that we cannot really do. We provide injections and do things we do not have education to do.”
(Consultant hospital B)
Healthcare professionals describe often asking the next of kin to observe the patient over time, report changes in the patient's condition, assist the patient with daily care, bring food or drinks to the patient, feed the patient, and share information that can prevent adverse events and enhance the quality of care. Next of kin are often a unique and invaluable resource for quality and safety of cancer care. One of the most appreciated features of next of kin involvement is the ability to motivate the patient and to share information about the patient.
…the most important contribution from next of kin is the dissemination of information at the doctor's or nurse consultations. […] Next of kin have a greater ability to understand because they are there for the patient while the patient has more than enough with himself.
(Manager, hospital B)
The division of work seems to come naturally because of the close relationship between the next of kin and the patient, but it also causes challenges. In both hospitals, there was confusion about what the next of kin could be asked to do and what role the next of kin should have in hospital cancer care. This is in contrast to the finding that the next of kin have a coordinating function in cancer care.
This result indicates that the hospital cancer care would benefit from a more systematic approach to next-of-kin involvement, enabling them to act promptly in light of the possible consequences of treatment and care by teaching them what to expect. Next-of-kin involvement may also strengthen the reflective processes around the patient by introducing viewpoints and observations that are not readily accessible to the health personnel, e.g., what the patient's life was like before the cancer diagnosis.